"Uncover the truth behind the groundbreaking discovery of the causes of the world's biggest problems. 'The Root Causes' will change how you view the world!"
Preventing and Managing IgA Nephropathy: A Comprehensive Approach
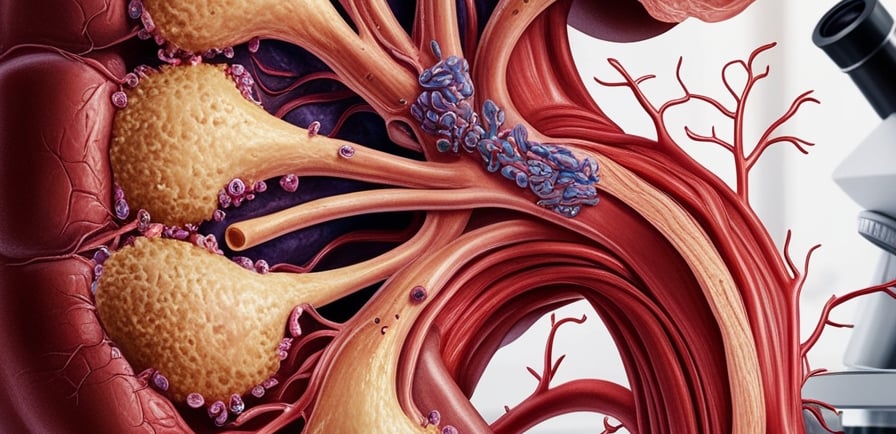
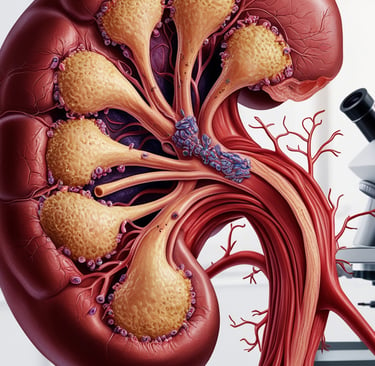
IgA Nephropathy (IgAN), also known as Berger's disease, is a kidney disorder characterized by the abnormal deposition of immunoglobulin A (IgA) antibodies in the glomeruli, leading to inflammation and potential kidney damage. Genetic mutations, particularly in genes like IGHA1 and IGHA2, along with environmental factors such as infections, play a significant role in disease progression. To slow IgAN’s progression, preventive strategies include managing blood pressure, avoiding oxidative stress, reducing calcium overload through dietary adjustments, and incorporating key supplements like magnesium, taurine, omega-3 fatty acids, and vitamins D, B12, and K2. Early diagnosis, medication adherence, and lifestyle changes such as a balanced diet, exercise, and smoking cessation are crucial for improving kidney health and preventing chronic kidney disease (CKD) and end-stage renal disease (ESRD).
DISEASES
Glenn Rosaroso Vale, BSMT, MS(IT), MBA
12/25/20245 min read
Preventing and Managing IgA Nephropathy (IgAN): A Comprehensive Approach
IgA Nephropathy (IgAN), also known as Berger’s disease, is one of the most common forms of glomerulonephritis, a condition where the glomeruli—the tiny filtering units of the kidneys—become inflamed and damaged. Over time, this can lead to chronic kidney disease (CKD) and even end-stage renal disease (ESRD) if left untreated. Understanding the root causes of IgAN, prevention strategies, and how to slow its progression is crucial for improving the quality of life for those affected by this disease.
The Root Cause of IgA Nephropathy
IgAN is primarily caused by the deposition of immunoglobulin A (IgA) antibodies in the kidneys’ glomeruli, which triggers an inflammatory response that damages the kidney tissue. However, the root causes of this abnormal immune response are multifaceted and involve genetic, environmental, and immunological factors.
Genetic Factors and Gene Mutations
Genetics plays a significant role in the development of IgAN. Research has identified specific gene mutations that increase susceptibility to the disease. Mutations in genes related to the immune system—particularly those involved in the mucosal immune response—are critical in the overproduction of abnormal IgA antibodies. These mutations can lead to an IgA antibody that is more prone to depositing in the glomeruli, triggering kidney damage.
Key genes implicated in IgAN include:
The IGHA1 and IGHA2 genes, which encode the immunoglobulin A antibodies.
Genes involved in the complement system, such as CFH (complement factor H), which helps regulate immune activity and prevents excessive activation that could contribute to kidney damage.
Family history is also a key risk factor. Individuals with a first-degree relative who has IgAN are at an increased risk of developing the disease, highlighting the hereditary nature of the condition. The exact genetic pathways are still being explored, but the presence of these mutations significantly predisposes individuals to IgAN.
Environmental and Immunological Factors
The immune system’s role in IgAN is complex. Typically, IgA antibodies are produced to protect mucosal surfaces like the respiratory and gastrointestinal tracts from infections. In IgAN, however, an abnormal form of IgA is produced, triggering inflammation and damage in the kidneys. Environmental factors, such as infections (especially respiratory and gastrointestinal), may further exacerbate this immune response in genetically predisposed individuals, contributing to the development and progression of the disease.
Prevention and Slowing Down the Progression of IgAN
While there is no cure for IgAN, various strategies can help prevent its progression and manage symptoms. Focusing on both lifestyle adjustments and addressing underlying genetic predispositions is key to slowing the disease's advancement.
1. Preventing Gene Mutation and Managing Risk Factors
While we cannot directly prevent genetic mutations, we can adopt strategies to limit environmental factors that trigger gene expression or accelerate disease progression:
Avoid Oxidative Stress: Oxidative stress can damage cells, including kidney cells, and worsen inflammation in IgAN. Antioxidants can help counteract this damage. To reduce oxidative stress, avoid toxins like cigarette smoke, pollution, and processed foods, which contribute to the production of free radicals.
Avoid Calcium Overload: Excess calcium in the body can contribute to kidney damage. Limiting carbohydrate intake to a maximum of 4 grams per meal, as recommended by Dr. Gay Fettke from Australia, can help prevent calcium overload by controlling insulin spikes that promote calcium retention. A low-carb diet, rich in healthy fats and proteins, can help maintain proper calcium balance and reduce kidney strain.
Minimize Exposure to Seed Oils and Toxins: Seed oils (such as those from sunflower, corn, and soy) and environmental toxins are inflammatory and can exacerbate kidney damage. A diet free from these processed oils and chemicals can help reduce oxidative stress and inflammation.
2. Dietary and Lifestyle Adjustments
Making key dietary and lifestyle changes is crucial for managing IgAN and preventing further kidney damage.
Dietary Modifications:
Low-Sodium, Low-Protein Diet: A low-sodium diet is essential for managing blood pressure and reducing strain on the kidneys. Reducing protein intake also helps prevent kidney damage from excess protein metabolism.
Balanced Macronutrients: Focus on a diet rich in lean proteins, such as fish and poultry, and healthy fats like olive oil and avocado. A low-carb approach, with careful portion control, can prevent insulin resistance and related complications.
High-Potassium Foods: Unless contraindicated due to elevated potassium levels, high-potassium foods such as leafy greens, bananas, and potatoes can help balance electrolytes and support kidney function.
Lifestyle Modifications:
Regular Exercise: Exercise helps manage blood pressure, improve circulation, and reduce inflammation. It’s important to tailor physical activity to individual health levels to avoid excessive strain.
Weight Management: Maintaining a healthy weight reduces the risk of conditions like diabetes and hypertension, which can exacerbate kidney damage in IgAN patients.
Avoid Smoking and Excessive Alcohol: Smoking and excessive alcohol consumption can accelerate kidney function decline. Quitting smoking and limiting alcohol intake are crucial steps in managing IgAN.
3. Supplementation to Support Kidney Health
Certain supplements can help manage the effects of IgAN by addressing calcium overload, oxidative stress, and immune system regulation:
Magnesium and Taurine: Both magnesium and taurine help reduce oxidative stress and balance calcium levels, providing important kidney protection.
Vitamins and Minerals:
Vitamin D, B1, B12, C, and K2: These vitamins support immune function, reduce inflammation, and help maintain kidney health.
Zinc: Zinc plays a critical role in immune system regulation and can reduce inflammatory responses.
Coenzyme Q10 (CoQ10): This antioxidant helps reduce oxidative stress and may improve kidney function.
Omega-3 Fatty Acids: Consuming Omega-3s through supplements or fatty fish like sardines and tuna can help reduce inflammation and support kidney health.
4. Blood Pressure Control and Medication Adherence
High blood pressure is a major contributor to kidney damage in IgAN. Managing hypertension is essential for slowing disease progression. Medications such as ACE inhibitors and angiotensin receptor blockers (ARBs) are commonly used to control blood pressure and reduce proteinuria, a key indicator of kidney damage.
In some cases, immunosuppressive drugs like corticosteroids or other agents may be prescribed to reduce the immune system's overactivity, preventing further IgA deposition in the kidneys.
5. Regular Monitoring and Follow-ups
Regular kidney function tests, including urine analysis and serum creatinine levels, are essential for tracking disease progression. Early intervention and treatment adjustments can help slow down the disease and improve long-term outcomes.
Current Research and Future Directions
Ongoing research into IgAN is focused on developing targeted therapies to reduce the abnormal IgA production or prevent its deposition in the kidneys. Biologic therapies and genetic treatments may provide new avenues for managing IgAN more effectively. Personalized medicine, tailored to an individual’s genetic makeup and immune response, is the future of IgAN treatment and could offer improved outcomes for patients.
Conclusion: A Holistic Approach to Managing IgA Nephropathy
IgA Nephropathy is a multifaceted disease that requires a comprehensive and proactive approach to management. By addressing the genetic, environmental, and immunological factors contributing to the disease, individuals can slow its progression and maintain kidney function. Early diagnosis, lifestyle adjustments, medication adherence, and supplementation can all play important roles in managing IgAN effectively.
Through continued research and a personalized treatment approach, there is hope for better outcomes and a potential cure in the future. By focusing on prevention strategies and making informed lifestyle choices, patients can improve their quality of life and reduce the risk of long-term kidney damage from IgAN.
Health
Understanding illness to empower your well-being journey.
Wellness
Knowledge
info@rootcauseprevention.com
903-268-6664
© 2024. All rights reserved.
grfv@sbcgloal.net