"Uncover the truth behind the groundbreaking discovery of the causes of the world's biggest problems. 'The Root Causes' will change how you view the world!"
Understanding Diabetic Retinopathy: Pathogenesis and Natural Synergistic Treatments
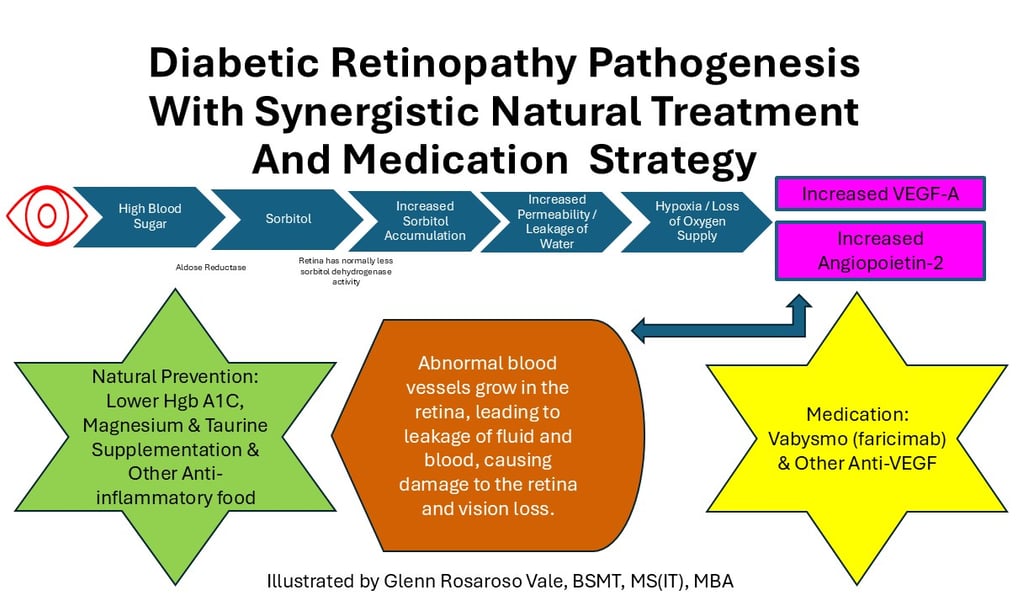
Diabetic retinopathy (DR) is a serious eye condition caused by prolonged high blood sugar, which leads to damage of the retinal blood vessels. This process involves the polyol pathway, where excess glucose is converted into sorbitol, accumulating in the retina due to limited breakdown, causing osmotic stress and inflammation. The increased intracellular calcium triggers the release of VEGF-A and Ang-2, which stimulate the growth of abnormal blood vessels, leading to leakage, edema, and potential vision loss. Effective management involves both medical treatments, such as injectable anti-VEGF medications like Vabysmo, and natural strategies, including controlling blood sugar (keeping HbA1c in check), reducing inflammation, and maintaining a healthy lifestyle to reduce the progression of DR and protect vision.
DISEASES
Glenn Rosaroso Vale, BSMT, MS(IT), MBA
12/20/20245 min read

Diabetic Retinopathy: Pathogenesis, Synergistic Natural Treatment, and Medication Prevention Strategy
Diabetic retinopathy (DR) is one of the most common and serious complications of diabetes, leading to vision impairment and blindness if left untreated. It is caused by damage to the blood vessels in the retina due to prolonged high blood sugar levels. While medical treatments such as injectable anti-VEGF medications are essential for managing this condition, natural preventive measures can play a critical role in slowing progression and maintaining retinal health. In this blog, we will explore the pathogenesis of diabetic retinopathy, focusing on the polyol pathway, and provide an effective combination of natural treatments and medication prevention strategies to combat this debilitating disease.
Pathogenesis of Diabetic Retinopathy
Diabetic retinopathy results from long-term exposure to high blood glucose levels, which can cause damage to the retinal blood vessels. The process begins at the cellular level, where elevated blood sugar triggers a series of biochemical pathways that lead to retinal damage and vision loss. One of the key mechanisms involved in this process is the polyol pathway, which plays a central role in the accumulation of sorbitol in the retina.
The Polyol Pathway and Sorbitol Accumulation
Under normal conditions, the body uses an enzyme called aldose reductase to convert excess glucose into sorbitol, a sugar alcohol. While this pathway helps with glucose regulation, it can become problematic in the context of uncontrolled diabetes. When blood sugar levels are persistently high, more glucose is directed into the polyol pathway. Sorbitol, however, has poor ability to pass through cell membranes and is not easily converted back into glucose.
In the retina, an area with minimal sorbitol dehydrogenase activity (the enzyme responsible for converting sorbitol into fructose), sorbitol cannot be efficiently broken down. As a result, sorbitol accumulates within retinal cells, leading to osmotic stress. The osmotic properties of sorbitol draw more water into the cells, including calcium ions, further increasing intracellular pressure.
Intracellular Calcium and Inflammation
The increased influx of calcium into retinal cells triggers a cascade of pathological reactions. One of the primary effects of excess intracellular calcium is the activation of various cellular pathways that lead to inflammation. This inflammation involves the production of pro-inflammatory cytokines, which contribute to swelling, oxidative stress, and endothelial cell dysfunction in the retina.
This inflammation damages the blood-retina barrier, reducing the oxygen supply to retinal tissues. As oxygen levels drop, the retina releases Vascular Endothelial Growth Factor (VEGF-A) and Angiopoietin-2 (Ang-2). These two molecules are key mediators of angiogenesis, the process of forming new blood vessels.
Angiogenesis and Retinal Damage
While angiogenesis is typically a repair mechanism in response to tissue injury, in diabetic retinopathy, it becomes dysregulated. The release of VEGF-A and Ang-2 leads to the growth of new, fragile, and leaky blood vessels in the retina. These abnormal blood vessels can cause fluid to leak into the surrounding tissues, leading to macular edema (swelling of the macula) and retinal hemorrhages. Over time, this results in vision loss, particularly central vision.
Synergistic Natural Treatment Approach
While medication plays a vital role in managing diabetic retinopathy, adopting a natural prevention strategy is essential to reduce the progression of the disease. A synergistic approach that combines lifestyle changes, dietary adjustments, and supplementation can complement medical treatments, offering a holistic method for maintaining retinal health.
1. Lowering HbA1c and Blood Sugar Levels
The cornerstone of preventing diabetic complications, including diabetic retinopathy, is optimal blood sugar control. One of the key markers for managing blood glucose over time is HbA1c. Keeping HbA1c levels in the normal range (less than 5.7%) can significantly reduce the risk of developing DR.
A natural strategy to achieve this involves:
Eating low-carbohydrate meals: Aim to consume no more than 4 grams of carbohydrates per meal. Focus on whole, unprocessed foods like leafy greens, lean proteins, healthy fats, and low-glycemic fruits.
Avoiding processed foods: Processed foods, especially those high in refined sugars and carbohydrates, can cause spikes in blood glucose levels. Eliminating processed foods is crucial for controlling blood sugar and preventing DR.
Using blood sugar monitoring: Regularly monitoring blood sugar levels and adjusting diet accordingly can help ensure steady control of glucose levels.
2. Regulating Intracellular Calcium and Reducing Inflammation
Managing the accumulation of intracellular calcium is critical for preventing the inflammatory cascade that leads to retinal damage. The following strategies can help:
Limiting carbohydrate intake: Excess carbohydrates, especially simple sugars and refined grains, contribute to elevated blood glucose and the polyol pathway. Reducing carbohydrate intake helps prevent the build-up of sorbitol and the resulting osmotic stress on retinal cells.
Avoiding seed oils and toxins: Seed oils (such as sunflower, canola, and soybean oils) are high in omega-6 fatty acids, which can promote inflammation. Opt for healthier fats, like those found in olive oil, avocados, and fatty fish.
Increasing antioxidants: Incorporate antioxidant-rich foods (like berries, nuts, and dark leafy greens) to combat oxidative stress and inflammation. Supplements like vitamin C, vitamin E, and zinc may also help support retinal health and reduce oxidative damage.
3. Maintaining a Healthy Lifestyle
Other lifestyle changes that can help reduce the risk and progression of diabetic retinopathy include:
Regular physical activity: Exercise helps improve insulin sensitivity, reducing the need for high amounts of insulin and helping to stabilize blood glucose levels.
Adequate hydration: Dehydration can exacerbate retinal damage. Ensure adequate fluid intake to support cellular function.
Stress management: Chronic stress can negatively affect blood sugar control. Practices such as meditation, yoga, or mindfulness can help manage stress and improve overall health.
Medication Strategy: Injectable Anti-VEGF Treatments
In conjunction with lifestyle changes, medication plays a crucial role in managing diabetic retinopathy. Anti-VEGF treatments target the underlying cause of abnormal blood vessel growth and leakage in the retina, helping to reduce the progression of the disease.
1. Vabysmo (Faricimab)
Vabysmo is a newly FDA-approved injectable medication that targets both VEGF-A and Angiopoietin-2 (Ang-2). By blocking these two proteins, Vabysmo prevents the abnormal blood vessel growth that causes retinal damage in diabetic retinopathy. It is administered via injection into the eye and can significantly reduce vision loss in patients with DR.
2. Other Anti-VEGF Injections
Other commonly used anti-VEGF medications include:
Lucentis (ranibizumab)
Eylea (aflibercept)
Beovu (brolucizumab)
Avastin (bevacizumab) – used off-label for retinal conditions
These medications work by inhibiting the effects of VEGF-A and, in some cases, other growth factors involved in angiogenesis, reducing the formation of abnormal blood vessels and leakage of fluid in the retina.
The Synergy Between Medication and Natural Prevention
While injectable anti-VEGF medications are effective in preventing vision loss due to diabetic retinopathy, their full potential is realized when paired with natural prevention strategies. Medications alone are not as effective if blood sugar levels remain poorly controlled or if the inflammation in the body is not addressed. Therefore, strict adherence to natural prevention measures, including diet and lifestyle changes, is crucial for the long-term success of diabetic retinopathy management.
Conclusion
Diabetic retinopathy is a serious complication of diabetes, but it is preventable and manageable with the right combination of medical treatment and natural prevention strategies. By focusing on blood sugar control, reducing inflammation, and using medications like anti-VEGF injections, you can significantly slow the progression of this disease and protect your vision. Combining these approaches offers the best chance of maintaining retinal health and preventing vision loss.
Health
Understanding illness to empower your well-being journey.
Wellness
Knowledge
info@rootcauseprevention.com
903-268-6664
© 2024. All rights reserved.
grfv@sbcgloal.net