"Uncover the truth behind the groundbreaking discovery of the causes of the world's biggest problems. 'The Root Causes' will change how you view the world!"
Understanding Atherosclerosis: The Role of High Blood Sugar and Seed Oils
The Development of Atherosclerosis: How High Blood Sugar and Seed Oils Contribute to Plaque Formation, and What We Can Do About It Atherosclerosis, commonly known as plaque buildup in the arteries, is a leading cause of heart disease, stroke, and other cardiovascular conditions. While genetic factors and lifestyle choices play a role, two often-overlooked contributors to the development of atherosclerosis are high blood sugar levels and the consumption of seed oils. These factors, when combined, create a dangerous cycle of cellular damage and inflammation, which ultimately leads to the formation of plaques in the blood vessels. In this blog post, we’ll explore how atherosclerosis develops, how high sugar and seed oils contribute to it, and what steps we can take to prevent or manage it. The Initial Trigger: Depolarization of the Cell Membrane When blood sugar levels exceed 90 mg/dL, the body activates specific enzymes, including aldose reductase, to process the excess glucose. Aldose reductase converts glucose into sorbitol through a process known as the polyol pathway. While this may seem like a natural defense mechanism, the accumulation of sorbitol creates osmotic pressure, which draws water into the cells. This water influx causes depolarization of the cell membrane, especially in endothelial cells lining the blood vessels. The depolarization of these cells has far-reaching consequences. As the cell membrane becomes unstable, it triggers an influx of calcium ions into the cell. This process, initiated by high sugar and compounded by the consumption of polyunsaturated fatty acids (PUFAs) found in seed oils, leads to a series of cascading events that damage the cells and tissues.
NUTRITIONDISEASES
Glenn Rosaroso Vale,DSMT, MS(IT), MBA
12/1/20246 min read
The Development of Atherosclerosis: How High Blood Sugar and Seed Oils Contribute to Plaque Formation, and What We Can Do About It
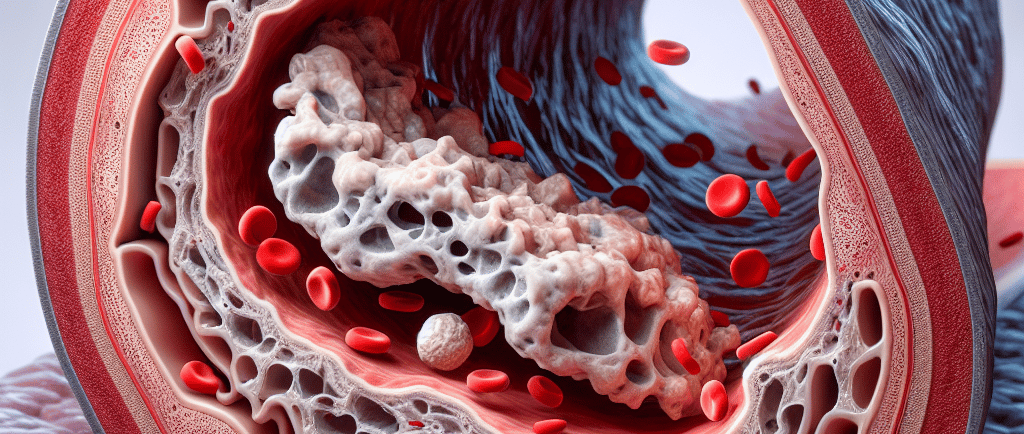
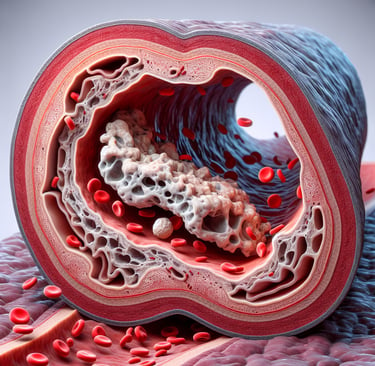
Atherosclerosis, commonly known as plaque buildup in the arteries, is a leading cause of heart disease, stroke, and other cardiovascular conditions. While genetic factors and lifestyle choices play a role, two often-overlooked contributors to the development of atherosclerosis are high blood sugar levels and the consumption of seed oils. These factors, when combined, create a dangerous cycle of cellular damage and inflammation, which ultimately leads to the formation of plaques in the blood vessels. In this blog post, we’ll explore how atherosclerosis develops, how high sugar and seed oils contribute to it, and what steps we can take to prevent or manage it.
The Initial Trigger: Depolarization of the Cell Membrane
When blood sugar levels exceed 90 mg/dL, the body activates specific enzymes, including aldose reductase, to process the excess glucose. Aldose reductase converts glucose into sorbitol through a process known as the polyol pathway. While this may seem like a natural defense mechanism, the accumulation of sorbitol creates osmotic pressure, which draws water into the cells. This water influx causes depolarization of the cell membrane, especially in endothelial cells lining the blood vessels.
The depolarization of these cells has far-reaching consequences. As the cell membrane becomes unstable, it triggers an influx of calcium ions into the cell. This process, initiated by high sugar and compounded by the consumption of polyunsaturated fatty acids (PUFAs) found in seed oils, leads to a series of cascading events that damage the cells and tissues.
The Role of Elevated Calcium Levels in Atherosclerosis
The elevation of intracellular calcium plays a central role in the pathogenesis of atherosclerosis. When blood sugar levels are high, they increase the production of uric acid, which leads to the formation of reactive oxygen species (ROS). These ROS cause oxidative stress, which further exacerbates the damage. This is where aldose reductase comes into play: it has a high Michaelis-Menten constant, meaning it is upregulated only when sugar concentrations are high. As a result, aldose reductase activity increases, leading to cellular damage and further disruption of cellular homeostasis.
The persistent elevation of calcium inside the endothelial cells causes mitochondrial dysfunction, reducing ATP production. This is significant because the endothelial cells play a crucial role in maintaining healthy blood vessels and regulating blood flow. When mitochondria are damaged, the endothelial cells cannot perform their functions efficiently, leading to a reduction in nitric oxide production and a loss of the glycocalyx, the protective lining of the blood vessel walls.
Calcium Overload and Smooth Muscle Contraction
As calcium accumulates inside the endothelial cells, it triggers additional problems. Calcium ions stimulate the release of more calcium from the endoplasmic reticulum (ER) into the cytosol, causing further elevation of intracellular calcium. This increased calcium influx activates voltage-gated calcium channels, which allows even more calcium to flow into the cells. The result is a vicious cycle of continuous calcium overload.
This excess calcium doesn't just affect the endothelial cells — it also impacts the smooth muscle cells in the walls of the blood vessels. When smooth muscle cells are exposed to high levels of calcium, they contract, leading to vasoconstriction, or the narrowing of blood vessels. This increases blood pressure, a condition known as hypertension.
High blood pressure, in turn, causes damage to the walls of the blood vessels, further impairing the glycocalyx and reducing nitric oxide production. As nitric oxide levels drop, inflammation is triggered, setting the stage for plaque formation in the arteries.
Calcium-Dependent Enzyme Upregulation and Thromboxane Production
An important aspect of calcium overload is the upregulation of calcium-dependent enzymes that play a role in inflammation and clotting. For example, the enzyme thromboxane synthase is highly regulated by calcium levels. When intracellular calcium rises, thromboxane synthase activity increases, leading to the production of thromboxane — a potent molecule that plays a key role in blood clotting.
Thromboxane promotes platelet aggregation and vasoconstriction, contributing to the development of blood clots. This is particularly relevant in the context of atherosclerosis, where plaque buildup in the arteries can rupture, triggering the clotting cascade. As thromboxane is produced in higher quantities due to elevated calcium levels, it amplifies the risk of heart attack or stroke by increasing the likelihood of clot formation in the blood vessels.
Plaque Formation: The Role of Inflammation and Cholesterol
As the blood vessels become more inflamed due to the reduction of nitric oxide, small, dense LDL cholesterol particles, along with calcium and monocytes (a type of white blood cell), infiltrate the blood vessel walls. The monocytes differentiate into macrophages and begin consuming oxidized LDL particles, which leads to the formation of foam cells — a hallmark of atherosclerosis.
These foam cells accumulate and form fatty streaks in the blood vessel walls. Over time, these streaks develop into plaques, which narrow and harden the arteries, limiting blood flow. As the plaques grow, they can eventually rupture, causing blood clots that may block blood flow entirely, resulting in heart attacks or strokes.
How High Sugar and Seed Oils Contribute to Atherosclerosis
The consumption of sugar and seed oils — particularly those high in omega-6 polyunsaturated fatty acids (PUFAs) — accelerates the development of atherosclerosis. Elevated blood sugar levels trigger the polyol pathway, leading to sorbitol accumulation and intracellular calcium overload, as discussed earlier. This process weakens the endothelial cells, reduces nitric oxide production, and causes inflammation, all of which are crucial steps in plaque formation.
Seed oils, on the other hand, are high in omega-6 fatty acids, which, when consumed in excess, contribute to chronic inflammation. The imbalance between omega-6 and omega-3 fatty acids in the body increases oxidative stress, which further damages the blood vessels and accelerates plaque buildup.
The Importance of Moderation in Carbohydrate Intake and Seed Oils
To mitigate the harmful effects of sugar, Dr. Gay Fettke, an Australian researcher, emphasizes that carbohydrate consumption must be strictly limited to 4 grams per meal. According to Dr. Fettke, controlling carbohydrate intake is essential to avoid sharp spikes in blood sugar, which can trigger the inflammatory and cellular damage processes that lead to atherosclerosis.
Furthermore, seed oil consumption should be kept to a minimal amount — about 0.6% of the Recommended Dietary Allowance (RDA) of omega-6 fatty acids. This is because excessive intake of seed oils contributes to inflammation and oxidative stress. Instead, it is recommended to use healthier oils such as coconut oil, olive oil, or avocado oil in cooking. Animal fats, including lard, also make for better choices due to their healthier fat profile, which supports overall cardiovascular health without triggering the same inflammatory responses as seed oils.
What Can We Do About It?
Now that we understand how high blood sugar and seed oils contribute to atherosclerosis, it’s essential to take proactive steps to prevent or manage this condition:
1. Reduce Sugar Intake
The most effective way to combat atherosclerosis is to maintain healthy blood sugar levels. This means reducing the intake of refined sugars and processed carbohydrates, which can spike blood glucose levels. Instead, focus on consuming whole, nutrient-dense foods such as vegetables, fruits, lean proteins, and whole grains. Following Dr. Gary Fettke's (2021) advice, keep your carbohydrate intake strictly to around 4 grams at a time.
2. Limit Seed Oils and PUFAs
Avoiding seed oils (such as sunflower, soybean, and canola oil) can help reduce the inflammatory effects caused by excessive omega-6 fatty acids. Keep your seed oil consumption minimal — no more than 0.6% of the RDA — and opt for healthier fat sources like olive oil, avocado oil, and coconut oil. Animal fats like lard are also a better alternative as they are less inflammatory.
3. Increase Omega-3 Fatty Acids
Omega-3 fatty acids, found in fatty fish like salmon, flaxseeds, and walnuts, can help balance the ratio of omega-6 to omega-3 fats in your diet. These healthy fats have anti-inflammatory properties that can reduce oxidative stress and support cardiovascular health.
4. Exercise Regularly
Physical activity helps regulate blood sugar levels, reduce inflammation, and improve overall heart health. Incorporating regular exercise into your routine can help prevent the development of atherosclerosis and reduce your risk of cardiovascular disease.
5. Maintain a Healthy Weight
Carrying excess weight, especially around the abdomen, can increase the risk of developing high blood sugar and hypertension. A balanced diet combined with regular exercise can help you maintain a healthy weight and prevent the onset of metabolic disorders that contribute to atherosclerosis.
Conclusion
Atherosclerosis is a complex process that begins with the damage to endothelial cells caused by high blood sugar and seed oils. This damage triggers inflammation, which leads to the accumulation of cholesterol and the formation of plaque in the arteries. By reducing sugar intake, avoiding seed oils, increasing omega-3s, and maintaining a healthy lifestyle, we can significantly reduce the risk of developing atherosclerosis and improve our cardiovascular health.
Understanding the mechanisms behind atherosclerosis empowers us to make informed choices and take control of our health, ultimately leading to a longer, healthier life.
Health
Understanding illness to empower your well-being journey.
Wellness
Knowledge
info@rootcauseprevention.com
903-268-6664
© 2024. All rights reserved.
grfv@sbcgloal.net