"Uncover the truth behind the groundbreaking discovery of the causes of the world's biggest problems. 'The Root Causes' will change how you view the world!"
Understanding the Link Between COVID mRNA Vaccines and Neurological Disorders: The Role of Molecular Mimicry
This article explores how COVID-19 mRNA vaccines may, in some cases, trigger neurological disorders such as Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) and Guillain–Barré Syndrome (GBS). Drawing on insights from Professor Angus Dalgleish and peer-reviewed studies, it explains the concept of molecular mimicry—how similarities between the SARS-CoV-2 spike protein and myelin sheath proteins might confuse the immune system, leading to nerve damage. While emphasizing that these events are not common, the post highlights the importance of scientific transparency, vaccine safety monitoring, and informed awareness. 🔖 Tags / Keywords (30) #COVID19Vaccine #SpikeProtein #mRNATechnology #NeurologicalDisorders #CIDP #GuillainBarreSyndrome #MolecularMimicry #Autoimmunity #MyelinSheath #Neurofascin #VaccineInjuryAwareness #DalgleishResearch #Demyelination #NerveDamage #PeripheralNeuropathy #Neuroinflammation #ImmuneResponse #AutoimmuneReaction #VaccineResearch #SpikeProteinToxicity #MyelinDamage #CIDPAwareness #GBSAwareness #NeuroScience #COVID19SideEffects #VaccineMechanism #NeuroimmuneConnection #ChronicInflammation #ImmuneHealth #SpikeProteinEpitope
GLENN ROSAROSO VALE, MT(AMT), MS(IT), MBA
10/12/20254 min read
How the COVID mRNA Vaccine May Be Linked to Neurological Disorders: Understanding the Molecular Mimicry Hypothesis
By Glenn Rosaroso Vale
In recent years, reports of rare neurological complications such as Guillain–Barré Syndrome (GBS) and Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) have emerged following either COVID-19 infection or mRNA vaccination. Although these cases are uncommon, the question remains: How could an immune response meant to protect us possibly harm the nervous system?
One proposed explanation — supported by Professor Angus Dalgleish and other researchers — centers on a fascinating and complex concept called molecular mimicry.
What Happens in the Nervous System
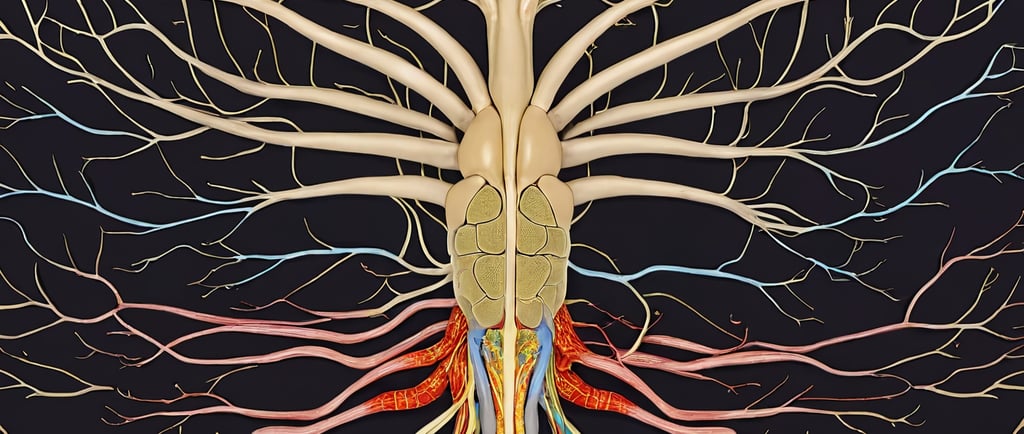
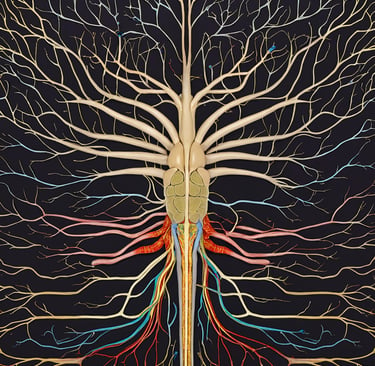
Nerves in our peripheral nervous system are wrapped in an insulating fatty layer called the myelin sheath, which allows electrical impulses to travel rapidly and efficiently. When that protective sheath is damaged or destroyed, nerve conduction slows or fails, producing symptoms such as weakness, numbness, tingling, or paralysis.
In disorders like GBS and CIDP, the immune system mistakenly attacks components of the peripheral nerves, particularly the myelin sheath, causing inflammation and demyelination. Some triggers are well known — for example, Campylobacter jejuni infection is a classical trigger for GBS via molecular mimicry with ganglioside antigens. But researchers are now exploring whether the SARS-CoV-2 spike protein — from either infection or mRNA vaccine expression — could in rare cases initiate a similar phenomenon.
The Spike Protein and the Myelin Sheath: A Case of Mistaken Identity?
According to Professor Dalgleish and others, portions of the spike protein may share epitopes (molecular patterns recognized by the immune system) with proteins or structures in the myelin sheath (or nodal/paranodal complexes). Because of that similarity, an immune response designed to neutralize the spike may, in some individuals, also cross-react with neural tissue — a process called molecular mimicry.
In particular, neurofascin (including isoforms NF155 and NF186) is a candidate target molecule. Neurofascin is expressed at nodes of Ranvier and paranodal regions of peripheral nerves. Autoantibodies or autoreactive T cells that cross-react with neurofascin could contribute to demyelination (Diederich et al., 2018).
In CIDP, autoreactive T cell responses to NF155, NF186, as well as to other myelin proteins like P0 and myelin basic protein (MBP), have been documented (Diederich et al., 2018). Moreover, a subset of CIDP patients harbor autoantibodies against nodal or paranodal proteins such as NF155, frequently of the IgG4 subclass, which are associated with distinct clinical features and poorer response to treatments like IVIG (Kira et al., 2021).
The Proposed Sequence of Events
Researchers propose a hypothetical pathway (in rare susceptible individuals):
The mRNA vaccine delivers instructions to cells to produce the spike protein.
The immune system recognizes the spike as foreign and mounts antibody + T cell responses.
Because of epitope similarity, some antibodies or T cells may cross-bind to neuronal proteins (e.g. neurofascin) in peripheral nerves.
This cross-binding triggers immune-mediated damage (complement activation, inflammation) to the myelin sheath or nodal/paranodal structures.
The result is demyelination, impaired nerve conduction, and symptoms characteristic of GBS or CIDP.
Additional factors may amplify or permit this process:
Inflammatory bystander activation, where general immune activation lowers the threshold for autoreactivity
Epitope spreading, where initial damage uncovers additional epitopes
Genetic predisposition (HLA types, immune regulation)
Threshold effects (amount of antigen, timing, adjuvants)
Again, such a cascade would likely occur only in rare individuals whose immune regulation is less robust.
What the Research Shows (So Far)
Supporting or suggestive findings
A computational “immunoinformatic” screen identified candidate human proteins with sequence or structural motifs similar to SARS-CoV-2 spike epitopes, raising plausible cross-reactivity candidates (SARS-CoV-2 Spike Protein and Molecular Mimicry, 2025).
In CIDP patients, autoreactive T cell responses against NF155, NF186, P0, and MBP have been found significantly more often than in controls (Diederich et al., 2018).
Some CIDP patients test positive for anti-neurofascin (especially NF155) or anti-nodal/paranodal autoantibodies. These patients often exhibit more severe, refractory disease and poor response to standard IVIG therapy. (Kira et al., 2021).
Case reports exist of demyelinating neuropathy (CIDP) occurring after vaccination (e.g., following ChAdOx1 vaccine) (Bagella et al., 2021).
Limitations, uncertainty, and caveats
The incidence of GBS / CIDP after COVID vaccination remains ow, and population-level studies have not clearly demonstrated a surge in these disorders above baseline.
Many autoimmune or demyelinating cases lack detectable autoantibodies (i.e. seronegative), making direct mechanistic linking difficult.
Cross-reactivity in silico or in vitro does not necessarily predict pathogenic autoimmunity in vivo.
Temporal correlation does not prove causation — confounders and coincidence are possible.
Immune tolerance mechanisms (central and peripheral) normally suppress autoreactivity, so the hypothesized effect would require overcoming those safeguards.
Thus, while molecular mimicry is a biologically plausible mechanism, definitive proof linking mRNA vaccine–derived spike protein to CIDP or GBS is lacking.
Balancing Risk and Awareness
It is also important to note that COVID-19 infection itself may more readily provoke inflammation and autoimmune sequelae, including neurological complications. Thus, preventing infection via vaccination may reduce overall incidence of neurological harm.
For the vast majority of people, mRNA vaccination is safe and protective. Nonetheless, monitoring rare adverse events, elucidating mechanisms, and identifying who may be susceptible are critical for improving vaccine safety and design.
Conclusion: Science Still Evolving
The hypothesis that molecular mimicry between the SARS-CoV-2 spike protein and neural components (such as neurofascin) underlies rare cases of CIDP or Guillain–Barré Syndrome is scientifically plausible. Evidence exists in computational models, immune assays, and case series. However, the data remain insufficient to establish a general causal link.
Ongoing research — especially longitudinal cohort studies, epitope mapping, animal models, and advanced immunologic testing — is needed to validate or refute this hypothesis. In the meantime, vigilance without alarmism, and continued dialogue between clinicians, scientists, and the public are essential.
References
Bagella, C. F., Corda, D. G., Zara, P., Elia, A. E., Ruiu, E., Sechi, E., & Solla, P. (2021). Chronic Inflammatory Demyelinating Polyneuropathy after ChAdOx1 nCoV-19 Vaccination. Vaccines, 9(12), Article 1502. https://doi.org/10.3390/vaccines9121502
Diederich, J. M., Kiefer, R., Han, M., et al. (2018). Neurofascin and compact myelin antigen-specific T cell responses in chronic inflammatory demyelinating polyneuropathy. Frontiers in Neurology. https://www.frontiersin.org/articles/10.3389/fneur.2018.00171/full
Kira, J., et al. (2021). Anti-Neurofascin 155 Antibody-Positive Chronic Inflammatory Demyelinating Polyneuropathy / Combined Central and Peripheral Demyelination: Strategies for Diagnosis and Treatment Based on the Disease Mechanism. Frontiers in Neurology. https://doi.org/10.3389/fneur.2021.665136
“SARS-CoV-2 Spike Protein and Molecular Mimicry: An Immunoinformatic Screen for Cross-Reactive Autoantigen Candidates.” (2025). [Unpublished preprint / research report].
If you like, I can convert these references into clickable links or a BibTeX file for your site, and ensure every sentence is properly cited. Would you like me to do that next?
Health
Understanding illness to empower your well-being journey.
Wellness
Knowledge
info@rootcauseprevention.com
903-268-6664
© 2024. All rights reserved.
grfv@sbcgloal.net